Αναπνευστική φυσικοθεραπεία
Breathing Pattern Disorders (BPD) - Leon Chaitow DO
BPD or Dysfunctional Breathing (DB)are abnormal respiratory patterns, most commonlyobserved in relation to over-breathing, which ranges from simple upper chest breathing to, at the extreme end of the scale, hyperventilation.
BPD/DBhas been defined as chronic or recurrent changes in breathing pattern that cannot be attributed to a specific medical diagnosis, causing respiratory and non-respiratory complaints.(Lum 1987).This is not a pathological process, but represents alterations in breathing patterns that interfere with normal physiological and metabolic functions.. BPD can co-exist with disease such as COPD or heart disease, and in some cases can mimic cardiac symptoms. (Sueda S et al. 2004, Ajani A 2007)
BPDs have been shown to destabilise mind, muscles, mood and metabolism. They commonly contribute tosymptoms experienced during premenstrual syndrome (Ott 2006).chronic fatigue(Nixon 1996),neck, back and pelvic pain(Smith et al 2006, Haugstad et al 2006)fibromyalgia (Naschitz J et al. 2006 , Dunnett A et al)and some aspects of anxiety and depression. (Lum 1987, Han et al 1996)
Epidemiology
It is estimated that approximately 10% of the population can be diagnosed with hyperventilation syndrome[12]. However, far more people have a more subtle, yet likely clinically significant, breathing pattern disorder. Dysfunctional breathing is more prevalent in women (14%) than in men (2%. (Thomas et al 2005). Preliminary data also suggest 5.3% or more of children with asthma also have dysfunctional breathing patterns, and that this is associated with poor asthma control.(Barker et al 2013)
Etiology
BPD occurs when ventilation exceeds metabolic demands, resulting in symptom-producing hemodynamic and chemical changes. Habitual failure to fully exhale - involving an upper chest breathing pattern - may result in hypocapnia where a deficiency of carbon dioxide CO2) in the blood occurs. This respiratory alkalosis, leads to hypoxia - the reduction of oxygen delivery to tissue. (Biff & Palmer 2012, Jensen 2004)
BPD also influences emotions(van Dixhoorn 2007),circulation, and digestive function - as well as musculoskeletal structures involved in the respiratory process. Essentially a sympathetic arousal ("fight-or-flight")develops. This frequently has negative effects on anxiety, blood pH, muscle tone, pain threshold, and a variety of central and peripheral nervous system symptoms. Therefore, despite not being an actual pathology, BPDs are produce symptoms that mimic pathological processes, such as cardiac and gastrointestinal problems.(Ajani A 2007)
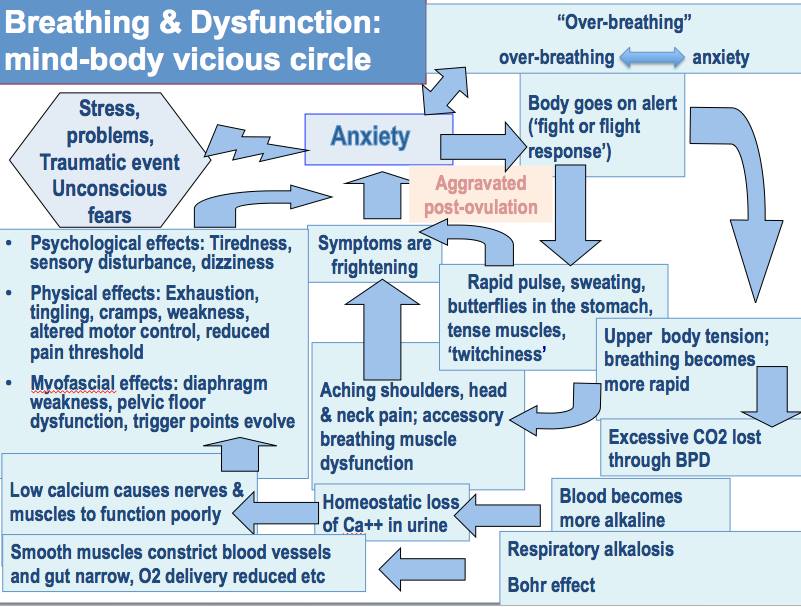
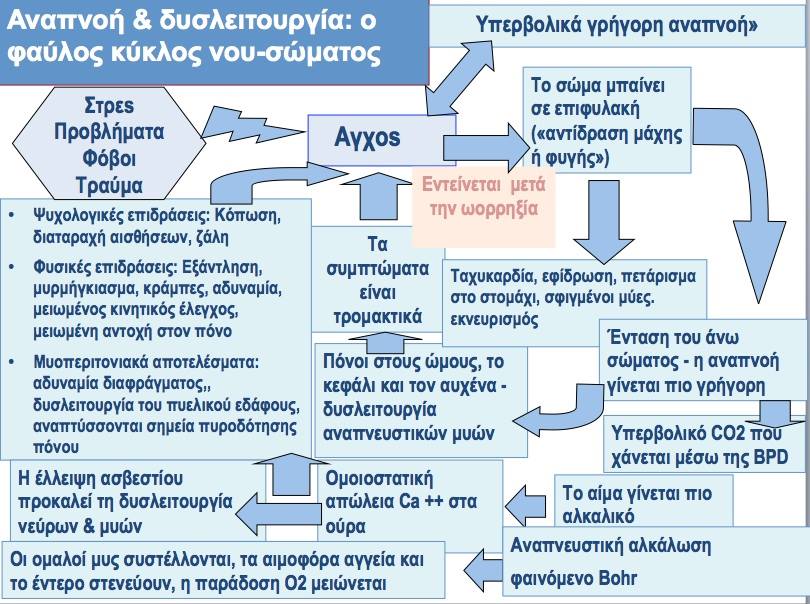
This diagram (from Chaitow et al 2014) demonstrates the multiple possible effects and influences of breathing pattern disorders.
Clinical Presentation
There are a wide variety of symptoms, the most extreme are shown in the diagram.
Typical symptoms can include:

• Frequent sighing and yawning
• Breathing discomfort
• Disturbed sleep
• Erratic heartbeats
• Feeling anxious
• Parasthesia
• Disturbed digestive function
• Clammy hands
• Chest Pains
• "Tired all the time"
• Aching muscles and joints – particularly in the neck, shoulder areas
• Dizzy spells
• Irritability or hypervigilance
• Feeling of 'air hunger'
Back Pain?
A correlation between BPD and low back pain has been suggested (Smith et al 2006)
Diagnostic Procedures
Nijmegan questionnaire
High scores on the Nijmegan questionnaire have been shown to be both sensitive and specific for detecting people with tendencies consistent with breathing pattern disorders. The sensitivity of the Nijmegen Questionnaire in relation to the clinical diagnosis was 91% and the specificity 95%. (van Dixhoorn J, Duivenvoorden 1985)
Assessment of breathing patterns
 • Breath Holding – People can normally hold their breath between 25 and 30 seconds. If less than 15 seconds suggests low tolerance to carbon dioxide possibly hrough habitual BPD..
• Breath Holding – People can normally hold their breath between 25 and 30 seconds. If less than 15 seconds suggests low tolerance to carbon dioxide possibly hrough habitual BPD..
• Observation: Seated or supine – hands on chest and stomach, while breathing normally – which hand moves first – and in what direction? Degree of lateral expansion is also observed.
• Seated Lateral Expansion – symmetrical lateral expansion is assessed. (Courtney et al 2008)
• Lung Plethysmography and Magnetometry
Assessment of musculoskeletal system
• Restricted movement of ribs, clavicle and diaphragm attachments.
• Excessive muscle tone and length especially involving psoas, quadratus lumborum, latissimus dorsi, upper trapezius, scalenes, and sternocleidomastoid
• Alterations in mobility of thoracic spine.
Assessment of respiratory function
• Oximetry - to measure oxygen saturation (SpO2)
• Capnography - to measure end tidal CO2 levels in exhaled air
• Peak expiratory flow rate
• Manual Assessment of Respiratory Motion -
Outcome Measures
• Nijmegen Questionnaire
• Rowley Breathing Self-Efficacy Scale (RoBE)
• Self Evaluation of Breathing Questionnaire (SEBQ)
• Hospital Anxiety and Depression Questionnaire (HAD)
Management / Interventions
Management ideally requires the removal of causative factors and the rehabilitation of habitual acquired dysfunctional breathing patterns. Restoration ofimproved or normal function of the respiratory system enhances rehabilitation - for example thoracic mobility and muscle tone and length.
Manual Therapy Techniques
 Based on your assessment, various manual therapy techniques that can be used to treat musculoskeletal imbalances and restrictions. These techniques include muscle energy techniques (MET), positional release, trigger point release and integrated neuromuscular inhibition techniques (Chaitow et al 2014)
Based on your assessment, various manual therapy techniques that can be used to treat musculoskeletal imbalances and restrictions. These techniques include muscle energy techniques (MET), positional release, trigger point release and integrated neuromuscular inhibition techniques (Chaitow et al 2014)
Breathing Retraining
• Awareness of faulty breathing patterns
• Relaxation of the jaw, upper chest, shoulders and accesssory respiratory muscles
• Abdominal/low-chest nose breathing pattern reeducation
• Awareness of normal breathing rates and rhythms, both at rest, during speech and activity.
Respiratory Techniques
• Pursed lip breathing to relieve dyspnoea, slow respiratory rate, increase tidal volume, and restore diaphragmatic function.
• Various additional strategies to reduce overactivity of accessory breathing muscles and to enhance diaphragmatic breathing
Complimentary methods
• Sleep retraining
• Relaxation
• Nutrition (to maintain normal blood-sugar levels)
• Capnography
Differential Diagnosis
BPDs can often mimic more serious conditions such as cardiac, neurological and gastrointestinal conditions which must all be ruled out by the medical team.
Bibliography
• Chaitow, L., Bradley, D. and Gilbert, C. 2014 Recognizing and Treating Breathing Disorders. Elsevier, 2014
• Bradley H, Dr Esformes J. 2014 Breathing pattern disorders and functional movement. Int J Sports Phys Ther. 2014 Feb;9(1):28-39.
• Barker NJ, Jones M, O'Connell NE, Everard ML 2013 .Breathing exercises for dysfunctional breathing/hyperventilation syndrome in children. Cochrane Database Syst Rev. 2013 Dec 18;12:CD010376.
• Jones M, Harvey A, Marston L, O'Connell NE. 2013 Breathing exercises for dysfunctional breathing/hyperventilation syndrome in adults. Cochrane Database Syst Rev. 2013 May 31;5:CD009041.
References
• Ajani A 2007 The mystery of coronary artery spasm Heart, Lung &; Circulation 16:10–15
• Barker, Nicola J et al. Breathing exercises for dysfunctional breathing/hyperventilation syndrome in children. National Library of Medicine. The Cochrane database of systematic reviews12 (2013): CD010376.
• Biff F. Palmer 2012 Evaluation and Treatment of Respiratory Alkalosis Am J Kidney Dis. 60(5):834-838.
• Chaitow, L., Bradley, D. and Gilbert, C. Recognizing and Treating Breathing Disorders. Elsevier, 2014
• Courtney R van Dixhoorn J Cohen M; Evaluation of Breathing Pattern: Comparison of a Manual Assessment of Respiratory Motion(MARM) and Respiratory Induction Plethysmography. Appl Psychophysiol Biofeedback (2008) 33:91–100
• Dunnett A et al. 2007 The diagnosis of fibromyalgia in women may be influenced by menstrual cycle phase. Journal of Bodywork and Movement Therapies 11:99-105
• Han J et al 1996 Influence of breathing therapy on complaints, anxiety and breathing pattern in patients with hyperventilation syndrome and anxiety disorders. J Psychosom Res. 41:481-493
• Haugstad G Haugstad T Kirste U 2006 Posture, movement patterns, and body awareness in women with chronic pelvic pain. J Psychosom Res. 61(5):637-644
• Jensen F 2004 Red blood cell pH, the Bohr effect, and other oxygenation-linked phenomena in blood O2 and CO2 transport Acta Physiologica Scandinavica 182(3):215-227
• Lum L 1987 Hyperventilation syndromes in medicine and psychiatry: a review. J. R Soc Med. 80:229-231.
• Peters, D. Foreword In: Recognizing and Treating Breathing Disorders. Chaitow, L., Bradley, D. and Gilbert, C. Elsevier, 2014
• Naschitz J et al. 2006 Patterns of hypocapnia on tilt in patients with fibromyalgia, chronic fatigue syndrome, nonspecific dizziness, and neurally mediated syncope. Am J Med Sci. 331:295-303
• Nixon P, Andrews J. 1996 A study of anaerobic threshold in chronic fatigue syndrome (CFS). Biol Psychol. 43:264
• Ott H et al 2006 Symptoms of premenstrual syndrome may be caused by hyperventilation Fertility and Sterility 86(4):1001.e17-1001.e19
• Smith M Russell A Hodges, P 2006. Disorders of breathing and continence have a stronger association with back pain than obesity and physical activity. Australian Journal of Physiotherapy 21(52):11-16
• Sueda S et al. 2004 Clinical impact of selective spasm provocation tests Coron Artery Dis 15(8):491–497
• Thomas M1, McKinley RK, Freeman E, Foy C, Price D.The prevalence of dysfunctional breathing in adults in the community with and without asthma. Prim Care Respir J. 2005 Apr;14(2):78-82.
• van Dixhoorn J 2007. Whole-Body breathing: a systems perspective on respiratory retraining. In: Lehrer P et al . (Eds.) Principles and practice of stress management. Guilford Press. NY pp. 291–332
• van Dixhoorn J, Duivenvoorden HJ. Efficacy of Nijmegen Questionnaire in recognition of the hyperventilation syndrome. J Psychosom Res. 1985;29(2):199-206.


Στην ίδια κατηγορία
-
ΙΛΙΓΓΟΣ ΑΥΧΕΝΙΚΗΣ ΑΙΤΙΟΛΟΓΙΑΣ
-
ΑΣΥΜΜΕΤΡΙΑ ΣΤΟ ΑΝΘΡΩΠΙΝΟ ΣΩΜΑ
-
ΖΩΗ ΣΗΜΑΙΝΕΙ ΚΙΝΗΣΗ, ΖΩΗ ΣΗΜΑΙΝΕΙ ΡΟΗ!
-
ΝΕΥΡΟΠΛΑΣΤΙΚΟΤΗΤΑ: Η ΙΚΑΝΟΤΗΤΑ ΤΟΥ ΕΓΚΕΦΑΛΟΥ ΝΑ ΑΝΑΔΙΑΜΟΡΦΩΝΕΤΑΙ
-
ΠΥΕΛΙΚΗ ΦΥΣΙΚΟΘΕΡΑΠΕΙΑ
-
ΠΑΙΔΙΑ ΚΑΙ ΔΙΑΔΙΚΤΥΟ: ΜΙΑ ΣΥΓΧΡΟΝΗ ΠΡΟΚΛΗΣΗ
-
ΧΕΙΡΟΘΕΡΑΠΕΙΑ vs ΗΛΕΚΤΡΟΘΕΡΑΠΕΙΑ ΣΤΟΝ ΑΥΧΕΝΙΚΟ ΠΟΝΟ
-
ΕΞΑΡΘΡΩΣΗ ΚΝΗΜΟΠΕΡΟΝΙΑΙΑΣ ΑΡΘΡΩΣΗΣ
-
STRESS: Η ΣΙΩΠΗΛΗ ΕΠΙΔΗΜΙΑ ΤΗΣ ΕΠΟΧΗΣ ΜΑΣ
-
ΑΜΜΕΣΗ ΠΡΟΣΒΑΣΗ ΣΤΗ ΦΥΣΙΚΟΘΕΡΑΠΕΙΑ – ΑΣΦΑΛΕΙΑ, ΑΠΟΤΕΛΕΣΜΑΤΙΚΟΤΗΤΑ ΚΑΙ ΘΕΣΜΙΚΕΣ ΠΡΟΫΠΟΘΕΣΕΙΣ
-
Η ΠΑΓΙΔΑ ΤΗΣ ΑΝΑΚΡΙΒΟΥΣ ΑΝΤΙΛΗΨΗΣ ΤΟΥ ΧΡΟΝΙΟΥ ΠΟΝΟΥ
-
MANUAL ALIGNMENT THERAPY: ΜΙΑ ΟΛΙΣΤΙΚΗ ΘΕΡΑΠΕΥΤΙΚΗ ΠΡΟΣΕΓΓΙΣΗ
Τελευταία άρθρα

ΙΛΙΓΓΟΣ ΑΥΧΕΝΙΚΗΣ ΑΙΤΙΟΛΟΓΙΑΣ
Ο ίλιγγος αυχενικής αιτιολογίας είναι μια σύνθετη κατάσταση που επηρεάζει την ισορροπία και την καθημερινή λειτουργικότητα των ασθενών.

ΑΣΥΜΜΕΤΡΙΑ ΣΤΟ ΑΝΘΡΩΠΙΝΟ ΣΩΜΑ
Η ιδέα τής συμμετρίας στο ανθρώπινο σώμα, είναι βαθιά ριζωμένη στη σκέψη μας ως συνώνυμο της υγείας και της σωστής στάσης. Στην πραγματικότητα όμως, το ανθρώπινο σώμα δεν είναι ούτε σχεδιασμένο, ούτε προορισμένο να είναι απόλυτα συμμετρικό.

ΖΩΗ ΣΗΜΑΙΝΕΙ ΚΙΝΗΣΗ, ΖΩΗ ΣΗΜΑΙΝΕΙ ΡΟΗ!
Η κίνηση αποτελεί θεμελιώδη μηχανισμό για τη ρύθμιση, προσαρμογή και διατήρηση τής λειτουργικότητας του σώματός μας.

ΝΕΥΡΟΠΛΑΣΤΙΚΟΤΗΤΑ: Η ΙΚΑΝΟΤΗΤΑ ΤΟΥ ΕΓΚΕΦΑΛΟΥ ΝΑ ΑΝΑΔΙΑΜΟΡΦΩΝΕΤΑΙ
Η νευροπλαστικότητα περιγράφει την ικανότητα του εγκεφάλου για συνεχή προσαρμογή, μάθηση και αποκατάσταση.

ΠΑΙΔΙΑ ΚΑΙ ΔΙΑΔΙΚΤΥΟ: ΜΙΑ ΣΥΓΧΡΟΝΗ ΠΡΟΚΛΗΣΗ
Στη σύγχρονη ψηφιακή εποχή μας, το διαδίκτυο προσφέρει στα παιδιά ευκαιρίες μάθησης και επικοινωνίας, αλλά και προκλήσεις για την ασφάλειά τους.

ΧΕΙΡΟΘΕΡΑΠΕΙΑ vs ΗΛΕΚΤΡΟΘΕΡΑΠΕΙΑ ΣΤΟΝ ΑΥΧΕΝΙΚΟ ΠΟΝΟ
Ποια θεραπευτική προσέγγιση προσφέρει την πιο αποτελεσματική και τεκμηριωμένη παρέμβαση στην αντιμετώπιση του αυχενικού πόνου;

ΕΞΑΡΘΡΩΣΗ ΚΝΗΜΟΠΕΡΟΝΙΑΙΑΣ ΑΡΘΡΩΣΗΣ
Η κνημοπερονιαία εξάρθρωση απαιτεί έγκαιρη διάγνωση και πρόγραμμα εξατομικευμένης αποκατάστασης για την λειτουργική επαναφορά τής άρθρωσης.

STRESS: Η ΣΙΩΠΗΛΗ ΕΠΙΔΗΜΙΑ ΤΗΣ ΕΠΟΧΗΣ ΜΑΣ
Το στρες αναδεικνύεται σε πολύπλευρη απειλή που διαβρώνει υγεία, ισορροπία και ποιότητα ζωής του σύγχρονου ανθρώπου.

ΑΜΜΕΣΗ ΠΡΟΣΒΑΣΗ ΣΤΗ ΦΥΣΙΚΟΘΕΡΑΠΕΙΑ – ΑΣΦΑΛΕΙΑ, ΑΠΟΤΕΛΕΣΜΑΤΙΚΟΤΗΤΑ ΚΑΙ ΘΕΣΜΙΚΕΣ ΠΡΟΫΠΟΘΕΣΕΙΣ
Η άμεση πρόσβαση στη φυσικοθεραπεία μπορεί να προσφέρει ασφαλή και ιδιαίτερα αποτελεσματική φροντίδα, ενισχύοντας την ποιότητα και την αποδοτικότητα των συστημάτων υγείας, ή εμπεριέχει κινδύνους για τους ασθενείς;

Η ΠΑΓΙΔΑ ΤΗΣ ΑΝΑΚΡΙΒΟΥΣ ΑΝΤΙΛΗΨΗΣ ΤΟΥ ΧΡΟΝΙΟΥ ΠΟΝΟΥ
Ο χρόνιος πόνος δεν αντικατοπτρίζει πάντα βλάβη ιστού, αλλά αφορά μια δυναμική κατάσταση με σύνθετους νευρολογικούς, ψυχολογικούς και κοινωνιολογικούς μηχανισμούς που απαιτούν κατανόηση και ολιστική προσέγγιση.