Treatment of carpal tunnel syndrome - non surgical approaches
Carpal tunnel syndrome (CTS) results from the entrapment of the median nerve at the wrist. It is the most common entrapment syndrome causing frequent disability especially to working populations. Aside from the surgical release approach there are other non-invasive therapeutic methods for the treatment of CTS. This paper will review the evidence regarding neurodynamic testing and neuromobilization of the median nerve as a treatment approach to CTS.
CLINICAL METHODS: NEURAL MOBILIZATION
Treatment of carpal tunnel syndrome: a review of the non-surgical approaches with emphasis in neural mobilization
Dimitrios Kostopoulos,
32-70 31st Street, Astoria, NY 11106, USA
Abstract
Carpal tunnel syndrome (CTS) results from the entrapment of the median nerve at the wrist. It is the most common entrapment syndrome causing frequent disability especially to working populations. Aside from the surgical release approach there are other non-invasive therapeutic methods for the treatment of CTS. This paper will review the evidence regarding neurodynamic testing and neuromobilization of the median nerve as a treatment approach to CTS.
Author Keywords: Carpal tunnel syndrome; Median nerve; Neural mobilization; Neurodynamic testing; Manual therapy
Introduction
Carpal tunnel syndrome (CTS) is the most common of all the nerve entrapment syndromes ([Phalen (1972)]). This syndrome is defined by the signs and symptoms resulting from compression of the median nerve at the wrist. CTS results in considerable discomfort and pain, limitation of activities of daily living, loss of sleep and work disability ( [Levine et al (1993)]). [Atroshi et al (1999a) and Atroshi et al (1999b)] identified that CTS in rather frequent in general population. Twenty percent of symptomatic subjects with symptoms of pain, numbness, and tingling in the hand, would be expected to have CTS based on clinical examination and electrophysiologic testing. [Papanicolaou et al (2001)] report that the lowest possible estimate of CTS prevalence in the general US population is 3.72%, indicating a larger pool of symptomatic people than previously reported.
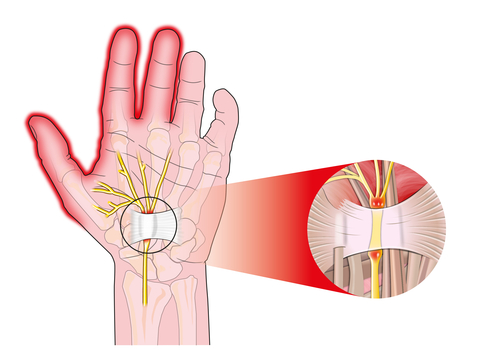
Anatomy
To achieve a better understanding on this entrapment syndrome we must first identify elements of the anatomy of the wrist and the tunnel formed by the carpal bones (Fig. 1). The carpus has a concave bony contour on its flexor surface and is covered by the flexor retinaculum. The bony carpus thus forms the floor and walls of the carpal tunnel, with the rigid flexor retinaculum as its roof. The flexor retinaculum, or transverse carpal ligament, attaches to the tubercle of the scaphoid, the ridge of the trapezium, and the ulnar aspect of the hook of the hamate and pisiform. The long flexors of the fingers and thumb pass through the carpal tunnel. The median nerve sits deep under the flexor retinaculum ([Snell (2000)]; [Primal Pictures (2001)]). It becomes superficial to the flexor digitorum superficialis muscle bellies just about 5 cm proximal to the transverse carpal ligament ([Szabo (1989)]). The median nerve is composed of 94% sensory fibers and only 6% motor fibers at the level of the carpal tunnel. However, the motor branch presents many anatomical variations, which create great variability of pathology in cases of CTS ( [Lanz (1977)]).

Figure 1. The wrist: carpal tunnel. Image courtesy of Primal Pictures Ltd. www.anatomy.tv ([Primal Pictures (2001)].
Etiology
The cause of compression of the median nerve at the carpal tunnel is the result of a discrepancy between the volume of the contents of the canal and its relative size ([Szabo (1989)]). [Gelberman et al (1981)] used a wick catheter to measure the intracarpal canal pressure in fifteen individuals suffering from CTS and in 12 control subjects. The mean pressure in the carpal canal was elevated significantly in the patients. When the wrist was in neutral position, the mean pressure was 32 mmHg. With 90° of wrist flexion the pressure increased to 94 mmHg, while with 90° of wrist extension the mean pressure was 110 mmHg. On the contrary the pressure in the control subjects with the wrist in neutral position was only 2.5 mmHg; with wrist flexion the pressure rose to 31 mmHg, and with wrist extension it increased to 30 mmHg. Carpal tunnel release brought about an immediate and sustained reduction in pressure. CT studies of patients with carpal tunnel syndrome show a decreased cross-sectional area of the carpal canal. Processes that can cause decreased volume or space within the carpal canal include tenosynovitis of the flexor tendons, Colles' fracture, and fracture-dislocation of the carpus and carpometacarpal joints. These processes may also cause posttraumatic scarring and/or fibrosis within the carpal tunnel. Inflammatory processes contributing to decreased volume within the carpal tunnel include rheumatoid arthritis, gout, pseudogout, amyloid deposition, and granulomatous infectious processes. All of these can produce a proliferative tenosynovitis with hyperplastic synovium. Tumors of the median nerve (e.g., neurilemomas, fibromas, and hamartomas) as well as tumors extrinsic to the median nerve (e.g., ganglia, lipomas, and hemangiomas) cause space-occupying encroachment of the carpal canal. Disorders that produce a volumetric increase within the carpal tunnel include acromegaly, hypothyroidism, pregnancy, diabetes mellitus, and lupus erythematosus. Volumetric increases are also seen in postmenopausal women. These systemic processes may increase extracapsular fluid retention and produce soft-tissue swelling. The carpal tunnel syndrome can thus be produced by compression or swelling of the median nerve in its synovial sheath ([Gelberman et al (1981)]; [Snell (2000)]; [Szabo (1989)]; [Primal Pictures (2001)]; [Rempel et al (1999)]).
Magnetic resonance scans on patients with non-specific arm pain (repetitive strain injury) show reduced median-nerve movement in the carpal tunnel, suggesting that this common condition may involve nerve entrapment ([Greening et al (1999)]). [Dilley et al (2001)] and [Greening et al (2001)] used ultrasound imaging to demonstrate reduced movement of the median nerve during wrist flexion in patients with non-specific arm pain. In 16 controls and 12 patients with non specific arm pain the position of the median nerve of the control subjects was 4.8 (SE=0.4) mm more radial with the wrist flexed than with the wrist extended while in the 12 arm pain patients the average change was only 1.2 (SE=0.5) mm. Both ultrasound imaging and magnetic resonance imaging confirm reduced nerve movement in patients with non-specific arm pain.
Diagnosis
Diagnosis for CTS can be rather challenging due to the great variability of symptomatology and the presence of both false positive, as well as false negative results of the various clinical and non-clinical diagnostic tests used. The clinical presentation usually is consistent with numbness and tingling in the median distribution of the hand. Sometimes the symptoms will be present only in one finger while in other cases the patient will complain of pain in the whole hand. In chronic cases symptoms are present above the carpal tunnel and may reach the cervical spine region. Thorough examination, including electrophysiology testing, of both the cervical spine and the wrist may reveal the presence of a double crush syndrome, involving compression of both the ipsilateral lower cervical nerve roots and the median nerve at the wrist ([Butler (1991) and Butler (2000)]; [Akalin et al (2002)]; [Maitland (2001)]; [Shacklock (1995)]). The literature on double crush pathology is rather confusing with some researchers denying the existence of this disorder ( [Bednarik et al (1999)]) and others who support it ( [Golovchinsky (1998)]; [Butler (1991) and Butler (2000)]; [Elvey (1997)]; [Shacklock (1995)]). Golovchinsky in his retrospective analysis of results of electromyography and nerve conduction velocity studies in 169 patients with lower back pain, identified peripheral entrapment of nerves (tarsal tunnel syndrome and anterior tarsal tunnel syndrome) in 5.3% of patients, signs of acute or chronic partial muscle denervation of corresponding muscles of lower extremities in 21.8% of patients, and abnormally prolonged F-wave latency in 12.5% of patients. Statistical analysis of his data showed significantly higher than random overlap of peripheral entrapment syndromes and signs of proximal nerve damage of the corresponding nerves. This higher than random coincidence of the two conditions strongly suggests cause-and-effect relationship of damage of the proximal stretch of motor nerve fibers and development of peripheral entrapment syndromes in the same nerves rather than a random coincidence of two independent pathologies ( [Golovchinsky (1998)]).
Physical examination for CTS may reveal findings related to decreased sensibility, abnormal response to provocative testing and/or decreased strength ([Szabo (1989)]). Sensibility tests include threshold tests, such as Semmes-Weinstein and vibrometry, as well as innervation density tests, such as two point discrimination tests. Provocative tests may include Phalen's, Tinel's and the tourniquet test ( [Szabo (1989)]). Additional provocation tests may include adverse neural tension tests for the median nerve ( [Butler (1991) and Butler (2000)]). Electrodiagnostic studies can provide a sensitive and objective testing procedure for the diagnosis of CTS ( [Dumitru et al (2002)]; [Kimura (1989)]; [Kraft and Halvorson (1983)]; [Szabo (1989)]). In patients with CTS there are usually electrophysiologic findings consistent with prolonged distal latency and delayed conduction velocity of either the sensory or motor component of the median nerve or even of both components as compared to normative data or to uninvolved nerves on the same patient ( [Kimura (1989)]; [Kraft and Halvorson (1983)]). Electromyographic studies of the thenar muscles can assist in the quantification of the severity of the condition. [Finsen and Russwurm (2001)] support that electrophysiology testing is not necessary as a pre-operative diagnostic tool for patients with typical CTS. In their research paper they examined 68 patients with typical carpal tunnel syndrome. Patients received electrophysiologic evaluations preoperatively, but these were not assessed until the end of their study. Open carpal tunnel release was performed and the clinical diagnosis of carpal tunnel syndrome was considered as confirmed when there was a prompt resolution of the preoperative symptoms. Sixty-three of the 68 patients responded well to surgery, three had equivocal outcomes and two did not improve, and thus were considered not to have carpal tunnel syndrome. The electrophysiological tests were normal in these two patients, but were also normal in 14 of the 63 patients who improved with carpal tunnel surgery. The authors support that preoperative electrophysiology testing might have led to up to 14 of the 63 cases of carpal tunnel syndrome being turned down for surgery. Thus, they concluded that electrophysiological testing contributes little to the diagnosis in typical cases of carpal tunnel syndrome ( [Finsen and Russwurm (2001)]). The researchers ignored to discuss the value of electrophysiological testing in terms of differential diagnosis in cases of CTS, therefore confirming the need or not of invasive intervention. This author believes that especially in cases of a double crush syndrome ( [Butler (1991) and Butler (2000)]), failure to recognize the degree of involvement of the cervical spine and administer appropriate treatment may lead to continuation of the distal symptoms post-operatively.
Treatment
Patients with long-lasting moderate or severe symptoms of CTS, especially when muscle weakness and atrophy are present, undergo carpal tunnel release. In some cases steroid injections into the carpal canal may offer temporary symptom relief. [Marshall et al (2002)] in an extensive review of the literature concerning injections in the carpal tunnel found that local corticosteroid injections provide greater clinical improvement in symptoms 1 month after injection compared to placebo. Symptom relief beyond 1 month compared to placebo has not been demonstrated. However, local corticosteroid injection provides significantly greater clinical improvement compared to oral steroid up to 3 months after treatment. [Marshall et al (2002)] and [O'Connor et al (2003)] searched the literature for studies in order to evaluate the effectiveness of non-surgical treatment (other than steroid injection) for carpal tunnel syndrome versus a placebo or other non-surgical, control interventions in improving clinical outcome. They found that current evidence shows significant short-term benefit from oral steroids, splinting, ultrasound, yoga and mobilization techniques of the carpal bones ( [O'Connor et al (2003)]). A recent randomized controlled study reported significant decrease of CTS symptoms after the application of red-beam laser (continuous wave, 15 mW, 632.8 nm) on shallow acupuncture points on the affected hand, infrared laser (pulsed, 9.4 W, 904 nm) on deeper points on upper extremity and cervical paraspinal areas, and microamps TENS on the affected wrist ([Naeser et al (2002)]). The effectiveness of nerve gliding (neuro-mobilization) treatments for CTS still remains controversial ( [Akalin et al (2002)]; [Jabre (1994)]; [Totten and Hunter (1991)]).
Neurodynamic testing
The idea of applying a mechanical treatment to the neural tissue is not new. Principles and methods of "nerve stretching" ([Symington (1882)]) existed since the late 1800s and by time became more refined both in theory and clinical application. During 1960s [Breig (1978)] introduced the term adverse mechanical tension in the central nervous system. Incorporation of this adverse mechanical neural tension with principles of clinical reasoning took place several years later ( [Maitland (1982)]). This work was further researched, expanded and presented to the clinical and scientific community by [Elvey (1979)] and [Butler (1991)]. The reasoning of the above clinical researchers is that multiple entrapment or compression sites of parts of the nervous system apply adverse mechanical tension in the nervous system affecting its overall mobility of and ability to transmit tension ( [Butler (2000)]; [Elvey (1997)]; [Maitland (2001)]). The examination processes of these physical abilities of the nervous system for mobility and transmission of tension are defined as "Neural Tension Tests" ( [Butler (1991) and Butler (2000)]). According to Shacklock the terms "Neural Tension Tests" or "Adverse Neural Tension Tests", which are extensively used by the clinical community, reflect the mechanical function and mechanical tension on the nervous system ( [Shacklock (1995)]). A more comprehensive term, "Neurodynamics", has been suggested by [Shacklock (1995)] to facilitate the inclusion of physiology, pathophysiology and pathomechanics in the mechanical treatment of the nervous system. The study of neurodynamics means the study of the mechanics and physiology of the nervous system and how they relate to each other ( [Shacklock (1995)]). The basic concept stipulates that in a normal mechanical and physiological state the nervous system will allow pain free movements and postures. In a pathological state pathomechanical and pathophysiological changes will induce a state of pathodynamics for the nervous system ( [Butler (2000)], [Shacklock (1999) and Shacklock (1995)]). So what is the answer to this state of pathodynamics for the nervous system? Since nerves are viscoelastic structures ( [Kwan (1992)]) they may respond to mobilization procedures and techniques ( [Shacklock (1995)]), similar to those for the musculoskeletal system, with purpose to correct such abnormal neural tensions and re-establish the proper movement of the neural tissue. This will result in a pain free state with subsequent improvement in the patient's functional ability level which is most of times the final goal. The basis of the ability of the nervous system for gliding and for transmission of tension has been thoroughly researched. Peripheral nerves have the ability to slide amongst other tissues and even slightly elongate ( [Butler (2000) and Butler (1991)]). Longitudinal sliding has been documented in highly reliable studies utilizing spectral Doppler ultrasonography. [Hough et al (2000a) and Hough et al (2000b)] and [McLellan and Swash (1976)] found that the median nerve slides longitudinally in its bed when the limb is moved. In cases of entrapment neuropathies, where longitudinal movement of a peripheral nerve is restricted, continual trauma results from normal movements of the limb.
[Byl et al (2002)] in cadaver studies researched the strain of the median nerve throughout upper-extremity positioning sequences used by clinicians to evaluate nerve dysfunction. They used a microstrain gauge to quantify strain and digital calipers to assess nerve excursion. Data analysis demonstrated that the median nerve tension test caused a maximum summative strain in the median nerve at the carpal tunnel of 7.6%, with the largest increase in strain during elbow extension (3.5%). Components of the median nerve tension test decreased strain in the ulnar nerve at the cubital tunnel. The researchers' findings support the use of upper-extremity positioning sequences in the clinic to induce nerve strain during evaluation of nerve dysfunction ( [Byl et al (2002)]).
The author of this article utilizes the following suggested sequencing for the most commonly used median nerve neurodynamic test
(i)Glenohumeral abduction.
(ii)Wrist extension.
(iii)Supination.
(iv)Glenohumeral lateral rotation.
(v)Elbow extension.
(vi)Neck lateral bending to opposite side.
This neurodynamic test can be considered positive if:
(i)It produces the patient's symptoms (pain, numbness, tingling).
(ii)There is asymmetry when testing right and left sides (limitation in range of motion, resistance in the movement, production of symptoms during movement).
(iii)Test responses altered by movement of distant body parts (neck).
In some cases localization of the entrapment or excessive tension can be possible while receiving continuous verbal feedback from the patient regarding his/her symptoms. An assessment can be made regarding involvement of the more distal or proximal part of the neural tissue. As the various testing components are added from the most distal part (wrist extension) to the most proximal part (cervical spine lateral flexion) a local increase of symptoms can be indicative of increased tension in the corresponding segment of the nerve.
Neural mobilization
When there is evidence of an entrapment of the median nerve at the wrist and there is a positive neurodynamic test, then neuromobilization techniques can be applied. These neuromobilization techniques include repetitive motions of the segment that produces the symptoms as well as combination of movements in the more distal and proximal segments. The treatment position used is identical to the testing position (see Figure 2, Figure 3, Figure 4 and Figure 5). The author of this paper utilizes a technique that includes 3 sets of 10 repetitions in each set, at a moderate pace and a 3 second hold at the final stretched position. If during neurodynamic testing, an assessment is made that a specific part of the nerve is more involved, the therapist may focus more in that segment of the nerve but always including all segments of the nerve in the technique respecting the continuity of the neural tissue. According to the author's experience, in the first few sessions all the neuromobilization treatment positions should happen passively. Therefore, the therapist may need the help of an assistant to facilitate the movement of the head for the mobilization of the proximal component of the nerve. As the treatments progress the therapist may include active patient movements in the various components of the maneuver.
Usual patient responses may include, a feeling of "stretching", tissue tension, light numbness, slight increase of pain symptoms during the technique. Such symptoms are usually reduced or eliminated immediately at the end of the procedure.
It is very important that a home exercise program is given to the patient and it should include self-mobilization techniques for the median nerve. The patient can assume the same arm and neck position while supporting his/her extended wrist against the wall. The home exercise technique can take place in standing or sitting position. The sequencing of movement is the same as previously described with the exception that the wrist extension is facilitated by placing the pre-extended wrist against the wall instead of the therapist facilitating such extension.
Research evidence
The limited research that exists regarding therapeutic outcomes is very promising. [Rozmaryn et al (1998)] treated 197 patients (240 hands) with CTS in two groups. Patients in both groups were treated by standard conservative methods, and those in one group were also treated with a program of nerve and tendon gliding exercises. Of those who did not perform the nerve and tendon gliding exercises, 71.2% underwent surgery compared with only 43.0% of patients who did perform them. Patients in the experimental group who did not undergo surgery were interviewed at an average follow-up time of 23 months. Of the 47 responders, 70.2% reported good or excellent results, 19.2% remained symptomatic, and 10.6% were non-compliant. The researchers concluded that a significant number of patients who would otherwise receive surgical intervention for failure of traditional conservative treatment can be spared the surgical morbidity of a carpal tunnel release ( [Rozmaryn et al (1998)]).
[Akalin et al (2002)] tested only 28 patients (36 hands) with the diagnosis of CTS and randomly assigned them to two groups. The patients were instructed to wear the splints all night and during the day as much as possible for 4 wk. The patients in group 2 were also instructed to perform series of nerve and tendon gliding exercises in addition to the splint treatment. At the end of treatment, statistically significant improvement was obtained in all parameters in both groups. The improvement in group 2 was slightly greater, but the difference between the groups was not significant. The nerve gliding protocol used in this study was very limited and applied by patients only as a home exercise program and not as a treatment intervention by a skilled professional.
Effectiveness of neuromobilization techniques is reported by several other researchers for the ulnar, radial and sciatic nerves ([Coppieters et al (1999) and Coppieters et al (2001)]; [Elvey (1997)]; [Jabre (1994)]; [Shacklock (1996)]; [Sweeney and Harms (1996)]; [Totten and Hunter (1991)]).
These treatment techniques should not be considered as a panacea for resolving all neuromusculoskeletal conditions. They have though a prominent place amongst the various manual therapy techniques and they could be part of a comprehensive and evidence-based manual therapy program.
Neurodynamics and neuromobilization is a relatively new field of manual therapy and its value and applications in CTS cases should be further explored with more controlled randomized studies focused not only in the mechanical and physiological responses of the neural tissue, but also in clinical outcome studies inclusive of implementation of neurodynamics and neuromobilization.
References
Akalin et al (2002). E. Akalin, O. El, O. Peker et al., Treatment of carpal tunnel syndrome with nerve and tendon gliding exercises. American Journal of Physical Medicine and Rehabilitation 81 (2002), pp. 108–113.
Atroshi et al (1999a). I. Atroshi et al., Prevalence of carpal tunnel syndrome in a general population. Journal of the American Medical Association 282 (1999), pp. 153–158.
Atroshi et al (1999b). I. Atroshi et al., Symptoms, disability, and quality of life in patients with carpal tunnel syndrome. Journal of Hand Surgery [Am] 24 (1999), pp. 398–404.
Bednarik et al (1999). J. Bednarik, Z. Kadanka and S. Vohanka, Median nerve mononeuropathy in spondylotic cervical myelopathy: double crush syndrome?. Journal of Neurology 246 (1999), pp. 544–551.
Breig (1978). A. Breig. Adverse Tension in the Central Nervous System: An Analysis of Cause and Effect. Relief by Functional Neurosurgery, Almqvist and Wiksel, Sweden (1978).
Butler (1991). D.S. Butler. Mobilisation of the Nervous System, Churchill Livingstone, Melbourne, Australia (1991).
Butler (2000). D.S. Butler. The Sensitive Nervous System, Noigroup Publications, Adelaide, Australia (2000).
Byl et al (2002). C. Byl, C. Puttlitz, N. Byl, J. Lotz and K. Topp, Strain in the median and ulnar nerves during upper-extremity positioning. Journal of Hand Surgery [Am] 27 (2002), pp. 1032–1040. Abstract | PDF (149 K)
Coppieters et al (1999). M.W. Coppieters et al., A qualitative assessment of shoulder girdle elevation during the upper limb tension test 1. Manual Therapy 4 (1999), pp. 33–38.
Coppieters et al (2001). M.W. Coppieters et al., Shoulder girdle elevation during neurodynamic testing: an assessable sign. Manual Therapy 6 (2001), pp. 88–96. Abstract | Abstract + References | PDF (406 K)
Dilley et al (2001). A. Dilley, J. Greening, B. Lynn et al., The use of cross-correlation analysis between high-frequency ultrasound images to measure longitudinal median nerve movement. Ultrasound in Medicine and Biology 27 (2001), pp. 1211–1218. Abstract | Full Text + Links | PDF (156 K)
Dumitru et al (2002). D. Dumitru, A.A. Amato and M. Zwarts. Electrodiagnostic Medicine (2nd Edition ed.),, Hanley & Belfus, Philadelphia (2002).
Elvey (1979). R.L. Elvey, Brachial plexus tension tests and the pathoanatomical origin of arm pain. In: E.F.T.L. Glasgow, Editor, Aspects of Amnipulative Therapy, Lincoln Institute of Health Sciences, Melbourne (1979), pp. 105–110.
Elvey (1997). R.L. Elvey, Physical evaluation of the peripheral nervous system in disorders of pain and dysfunction. Journal of Hand Therapy 10 (1997), pp. 122–129.
Finsen and Russwurm (2001). V. Finsen and H. Russwurm, Neurophysiology not required before surgery for typical carpal tunnel syndrome. Journal of Hand Surgery
26 (2001), pp. 61–64. Abstract | Abstract + References | PDF (116 K)
Gelberman et al (1981). R.H. Gelberman, P.T. Hergenroeder, A.R. Hargens et al., The carpal tunnel syndrome. A study of carpal canal pressures. Journal of Bone and Joint Surgery [Am] 63 (1981), pp. 380–383.
Golovchinsky (1998). V. Golovchinsky, Double crush syndrome in lower extremities. Electromyography and Clinical Neurophysiology 38 (1998), pp. 115–120.
Greening et al (1999). J. Greening, S. Smart, R. Leary et al., Reduced movement of median nerve in carpal tunnel during wrist flexion in patients with non-specific arm pain. Lancet 354 (1999), pp. 217–218. Abstract | Full Text + Links | PDF (67 K)
Greening et al (2001). J. Greening, B. Lynn, R.M. Leary et al., The use of ultrasound imaging to demonstrate reduced movement of the median nerve during wrist flexion in patients with non-specific arm pain. Journal of Hand Surgery
26 (2001), pp. 401–406 (discussion 407–8) . Abstract | Abstract + References | PDF (395 K)
Hough et al (2000a). A.D. Hough, A.P. Moore and M.P. Jones, Measuring longitudinal nerve motion using ultrasonography. Manual Therapy 5 (2000), pp. 173–180. Abstract | Abstract + References | PDF (381 K)
Hough et al (2000b). A.D. Hough, A.P. Moore and M.P. Jones, Peripheral nerve motion measurement with spectral Doppler sonography: a reliability study. Journal of Hand Surgery
25 (2000), pp. 585–589. Abstract | Abstract + References | PDF (227 K)
Jabre (1994). J.F. Jabre, "Nerve rubbing" in the symptomatic treatment of ulnar nerve paresthesia. Muscle and Nerve 17 (1994), p. 1237.
Kimura (1989). J. Kimura. Electrodiagnosis in Diseases of Nerve and Muscle: Principles and Practice, F.A.Davis Co, Philadelphia (1989).
Kraft and Halvorson (1983). G.H. Kraft and G.A. Halvorson, Median nerve residual latency: normal value and use in diagnosis of carpal tunnel syndrome. Archives of Physical Medicine and Rehabilitation 64 (1983), pp. 221–226.
Kwan (1992). M. Kwan, Strain, stress and stretch of peripheral nerve: rabbit experiments in vitro and in vivo. Acta Orthopaedica Scandinavica 63 3 (1992), pp. 267–272.
Lanz (1977). U. Lanz, Anatomical variations of the median nerve in the carpal tunnel. Journal of Hand Surgery [Am] 2 (1977), pp. 44–53.
Levine et al (1993). D.W. Levine, B.P. Simmons, M.J. Koris et al., A self-administered questionnaire for the assessment of severity of symptoms and functional status in carpal tunnel syndrome. Journal of Bone and Joint Surgery [Am] 75 (1993), pp. 1585–1592.
Maitland (1982). G.D. Maitland, Examination of the cervical spine. Australian Journal of Physiotherapy 28 (1982), p. 6.
Maitland (2001). G.D. Maitland. Maitland's Vertebral Manipulation (6th Edition ed.),, Butterworth-Heinemann, Woburn, MA (2001).
Marshall et al (2002). Marshall, S., Tardif, G., Ashworth, N., 2002. Local corticosteroid injection for carpal tunnel syndrome. Cochrane Database System Reviews CD001554.
McLellan and Swash (1976). D.L. McLellan and M. Swash, Longitudinal sliding of the median nerve during movements of the upper limb. Journal of Neurology Neurosurgery and Psychiatry 39 (1976), pp. 566–570.
Naeser et al (2002). M.A. Naeser, K.A. Hahn, B.E. Lieberman and K.F. Branco, Carpal tunnel syndrome pain treated with low-level laser and microamperes transcutaneous electric nerve stimulation: a controlled study. Archives of Physical Medicine and Rehabilitation 83 (2002), pp. 978–988. Abstract | PDF (96 K)
O'Connor et al (2003). O'Connor, D., Marshall, S., Massy-Westropp, N., 2003. Non-surgical treatment (other than steroid injection) for carpal tunnel syndrome. Cochrane Database System Reviews CD003219.
Papanicolaou et al (2001). G.D. Papanicolaou, S.J. McCabe and J. Firrell, The prevalence and characteristics of nerve compression symptoms in the general population. Journal of Hand Surgery [Am] 26 (2001), pp. 460–466. Abstract | Full Text + Links | PDF (58 K)
Phalen (1972). G.S. Phalen, The carpal-tunnel syndrome, clinical evaluation of 928 hands. Clinical Orthopedics 83 (1972), pp. 29–40.
Primal Pictures (2001). Primal Pictures. 2001. Primal 3D Interactive Series: Hand. Primal Pictures Ltd.
Rempel et al (1999). D. Rempel, L. Dahlin and G. Lundborg, Pathophysiology of nerve compression syndromes: response of peripheral nerves to loading. Journal of Bone and Joint Surgery [Am] 81 (1999), pp. 1600–1610.
Rozmaryn et al (1998). L.M. Rozmaryn, S. Dovelle, E.R. Rothman et al., Nerve and tendon gliding exercises and the conservative management of carpal tunnel syndrome. Journal of Hand Therapy 11 (1998), pp. 171–179.
Shacklock (1995). M.O. Shacklock. Moving in on Pain, Butterworth-Heinemann, Australia (1995).
Shacklock (1996). M.O. Shacklock, Positive upper limb tension test in a case of surgically proven neuropathy: analysis and validity. Manual Therapy 1 (1996), pp. 154–161. Abstract | PDF (1150 K)
Shacklock (1999). M.O. Shacklock, The clinical application of central pain mechanisms in manual therapy. Australian Journal of Physiotherapy 45 (1999), pp. 215–221.
Snell (2000). R.S. Snell. Clinical Anatomy for Medical Students, Lippincott Williams & Wilkins, Baltimore, MD (2000).
Sweeney and Harms (1996). J. Sweeney and A. Harms, Persistent mechanical allodynia following injury of the hand. Treatment through mobilization of the nervous system. Journal of Hand Therapy 9 (1996), pp. 328–338.
Symington (1882). J. Symington, The physics of nerve stretching. British Medical Journal May 27 (1882), pp. 770–771.
Szabo (1989). R.M. Szabo. Nerve Compression Syndromes. Diagnosis and Treatment, Slack Inc, Thorofare, NJ (1989).
Totten and Hunter (1991). P.A. Totten and J.M. Hunter, Therapeutic techniques to enhance nerve gliding in thoracic outlet syndrome and carpal tunnel syndrome. Hand Clinics 7 (1991), pp. 505–520.
Στην ίδια κατηγορία
-
ΔΙΑΤΑΡΑΧΗ ΣΤΗ ΣΤΑΣΗ ΤΟΥ ΣΩΜΑΤΟΣ
-
ΚΡΑΝΙΟΪΕΡΗ ΘΕΡΑΠΕΙΑ ΓΙΑ ΤΗΝ ΗΜΙΚΡΑΝΙΑ (ΕΡΕΥΝΑ)
-
ΑΤΛΑΝΤΟ-ΙΝΙΑΚΗ ΕΝΩΣΗ: Mια αµφίδροµη σχέση
-
ΟΣΤΕΟΡΘΡΙΤΙΔΑ ΚΑΙ ΣΥΝΤΗΡΗΤΙΚΗ ΘΕΡΑΠΕΙΑ
-
ΠΡΩΙΜΗ ΕΝΑΡΞΗ ΦΥΣΙΚΟΘΕΡΑΠΕΙΑΣ ΣΤΗΝ ΟΣΦΥΑΛΓΙΑ
-
ΣΥΝΔΡΟΜΟ ΘΩΡΑΚΙΚΗΣ ΕΞΟΔΟΥ - Ανασκόπηση
-
Η ΜΑΧΗ ΕΝΑΝΤΙΑ ΣΤΗ ΒΑΡΥΤΗΤΑ
-
ΣΤΑΔΙΑ ΤΗΣ ΜΑΘΗΣΗΣ
-
TENSEGRITY: ΔΥΝΑΜΙΚΗ ΕΥΕΛΙΞΙΑ ΓΙΑ ΤΟΝ ΑΝΡΘΡΩΠΟ
-
ΕΞΕΡΕΥΝΩΝΤΑΣ ΤΟΝ ΠΟΝΟ ΣΤΟΝ ΓΛΟΥΤΟ (ΙΣΧΙΑΚΟ ΝΕΥΡΟ)
-
ΑΣΥΜΜΕΤΡΙΑ | ΑΛΛΑΓΗ ΣΤΗΝ ΕΥΘΥΓΡΑΜΜΙΣΗ ΤΟΥ ΣΚΕΛΕΤΟΥ
-
ΙΣΟΡΡΟΠΙΑ ΚΑΙ ΙΔΑΝΙΚΗ ΣΤΑΣΗ ΤΟΥ ΣΩΜΑΤΟΣ
Τελευταία άρθρα
-

ΔΙΑΤΑΡΑΧΗ ΣΤΗ ΣΤΑΣΗ ΤΟΥ ΣΩΜΑΤΟΣ
| Χαράλαμπος Τιγγινάγκας MSc | ΣκέψειςΗ διαταραχή τής στάσης μπορεί να θεωρηθεί ως θέμα των ιστών εξαιτίας τάσης, τραύματος, ή συνδρόμου καταπόνησης, αλλά τελικά είναι ενδεικτικό ανεπάρκειας στο λειτουργικό –software- τού εγκεφάλου.
-

ΚΡΑΝΙΟΪΕΡΗ ΘΕΡΑΠΕΙΑ ΓΙΑ ΤΗΝ ΗΜΙΚΡΑΝΙΑ (ΕΡΕΥΝΑ)
| Χαράλαμπος Τιγγινάγκας MSc | Πονοκέφαλος - ΗμικρανίεςΗ αντιμετώπιση της ημικρανίας είναι ένα σοβαρό πρόβλημα που απασχολεί ιδιαίτερα τόσο τους ασθενείς, όσο και τους επιστήμονες υγείας.
-

ΟΣΤΕΟΡΘΡΙΤΙΔΑ ΚΑΙ ΣΥΝΤΗΡΗΤΙΚΗ ΘΕΡΑΠΕΙΑ
| Χαράλαμπος Τιγγινάγκας MSc | ΟστεοαρθρίτιδαΗ οστεοαρθρίτιδα αποτελεί μια σύνθεση βιολογικών, γενετικών και περιβαλλοντικών παραγόντων. Η εμβάθυνση στην επιστημονική κατανόηση της νόσου είναι κρίσιμη για τη βελτίωση της ποιότητας ζωής των ασθενών.
-

ΠΡΩΙΜΗ ΕΝΑΡΞΗ ΦΥΣΙΚΟΘΕΡΑΠΕΙΑΣ ΣΤΗΝ ΟΣΦΥΑΛΓΙΑ
| Χαράλαμπος Τιγγινάγκας MSc | ΣκέψειςΣτην οσφυαλγία και την ισχιαλγία, η πρώιμη έναρξη φυσικοθεραπευτικού προγράμματος αποκατάστασης είναι κρίσιμη για την αποτελεσματικότητα της θεραπείας.
-

ΣΥΝΔΡΟΜΟ ΘΩΡΑΚΙΚΗΣ ΕΞΟΔΟΥ - Ανασκόπηση
| Χαράλαμπος Τιγγινάγκας MSc | Σύνδρομο Θωρακικής εξόδουΤο σύνδρομο θωρακικής εξόδου είναι μία από τις πιο αμφιλεγόμενες κλινικές καταστάσεις στην ιατρική.
-

Η ΜΑΧΗ ΕΝΑΝΤΙΑ ΣΤΗ ΒΑΡΥΤΗΤΑ
| Χαράλαμπος Τιγγινάγκας MSc | Στάση σώματος / ΛειτουργικότηταΟι επιπτώσεις από την δύναμη της βαρύτητας είναι συνδεδεμένες με τις αλλαγές στην ευθυγράμμιση του σκελετού και την εμφάνιση του πόνου. Η σωστή λειτουργία τού εγκεφάλου μάς προφυλάσσει, για άλλη μια φορά!
-

ΣΤΑΔΙΑ ΤΗΣ ΜΑΘΗΣΗΣ
| Χαράλαμπος Τιγγινάγκας MSc | Πληροφορίες για τον ΕγκέφαλοΗ γνώση είναι ζωτικής σημασίας για τη σύγχρονη κοινωνία. Σε αντίθεση με τους προγόνους μας, ο κόσμος μας εκτιμά τη διανοητική ικανότητα πολύ περισσότερο από τη σωματική ικανότητα και έτσι η ανάγκη απόκτησης γνώσεων είναι πλέον ύψιστης σημασίας.
-
TENSEGRITY: ΔΥΝΑΜΙΚΗ ΕΥΕΛΙΞΙΑ ΓΙΑ ΤΟΝ ΑΝΡΘΡΩΠΟ
| Χαράλαμπος Τιγγινάγκας MSc | Manual TherapyΤα φορτία και οι δυνάμεις συμπίεσης που δέχεται το σώμα, κατανέμονται ομοιόμορφα χάρη στο δυναμικό σύστημα tensegrity αντιβαρυτικής τάσης. Αυτό το μοντέλο θέλει τη θέση και τη στάση των οστών να εξαρτώνται κυρίως από την ισορροπία μεταξύ των μαλακών ιστών, αποδυναμώνοντας οποιαδήποτε χειρισμό ανάταξης για την επαναφορά της σωστής "ευθυγράμμισης".
-

ΕΞΕΡΕΥΝΩΝΤΑΣ ΤΟΝ ΠΟΝΟ ΣΤΟΝ ΓΛΟΥΤΟ (ΙΣΧΙΑΚΟ ΝΕΥΡΟ)
| Χαράλαμπος Τιγγινάγκας MSc | ΙσχιαλγίαΣτον γλουτό έχουν αποδοθεί περισσότερα σύνδρομα από οποιαδήποτε άλλη περιοχή του σώματος.
-

ΑΣΥΜΜΕΤΡΙΑ | ΑΛΛΑΓΗ ΣΤΗΝ ΕΥΘΥΓΡΑΜΜΙΣΗ ΤΟΥ ΣΚΕΛΕΤΟΥ
| Χαράλαμπος Τιγγινάγκας MSc | Manual TherapyΗ ελαχιστοποίηση των ασυμμετριών βελτιστοποιεί τη μηχανική τού σώματος και αποτρέπει, μελλοντικά, σοβαρά προβλήματα πόνου.